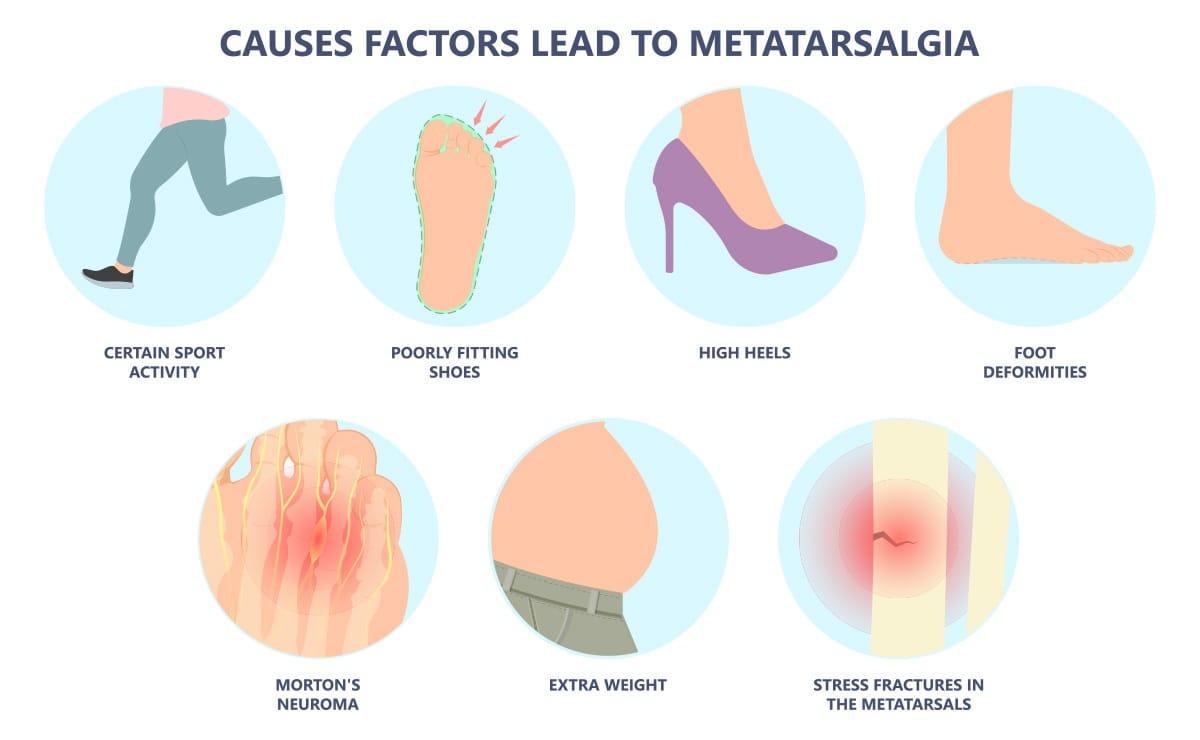
Many factors can contribute to the development of metatarsalgia, including those beyond our control, such as genetics and foot structure, as well as factors within our control, such as footwear and physical activity.
Identifying and understanding the cause is essential for successful treatment.
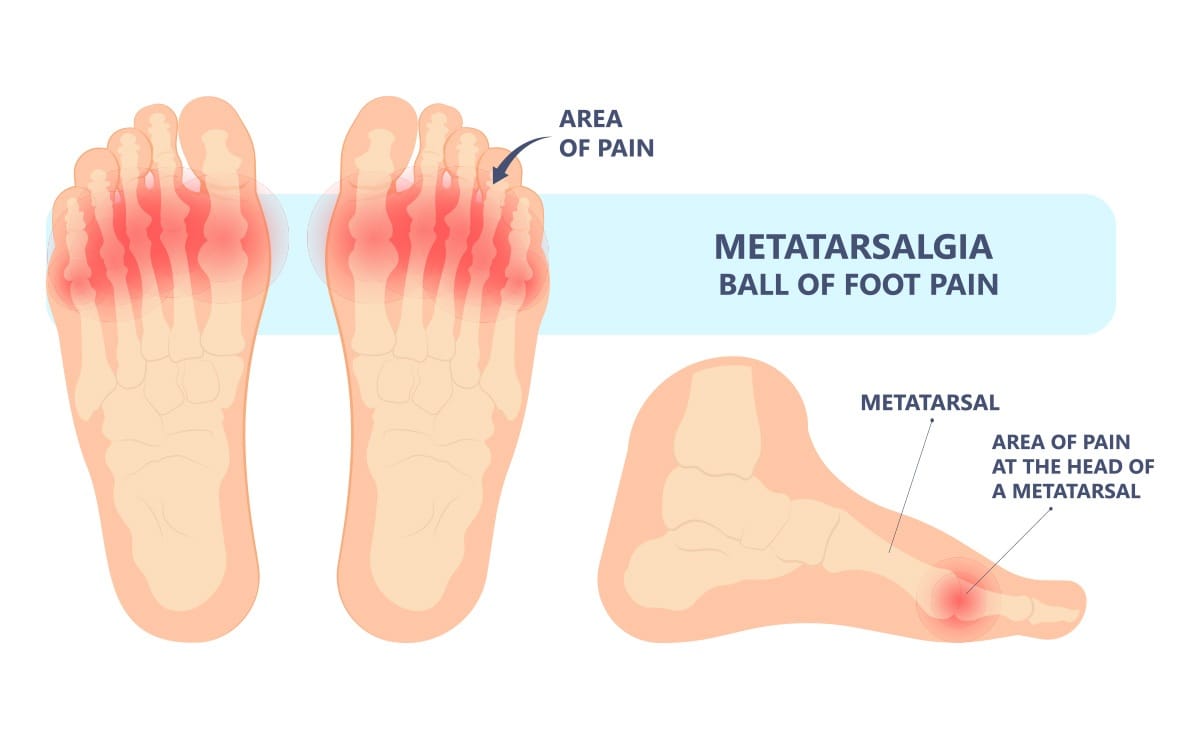
Common issues of the foot that may result in metatarsalgia:
Foot Deformities:
- Bunions (Hallux Valgus): A bunion changes the function of the first metatarsal and the foot, causing the other metatarsals to bear more weight.
- Hammertoes or Claw Toes: Toe deformities cause a retrograde pressure, pushing the ball of the foot downward, making the area more prominent and increasing pressure.
- High Arches (Pes Cavus): Feet with very high arches have prominent metatarsal areas, leading to increased pressure in the area.
- Flat Feet (Pes Planus): Flat feet can sometimes be less stable and lead to increased pressure in the forefoot.
- A long second metatarsal: If the second metatarsal is longer than the first metatarsal, it can cause increased pressure in the metatarsal area.
- Morton’s Neuroma: This condition involves inflammation around one of the nerves from the ball of the foot to the toes. Symptoms include sharp, burning pain and numbness in the ball of the foot and toes, increasing with activity.
- Stress Fractures: Excessive pressure on the metatarsals can cause the bone to weaken and develop a fracture. This is often due to overuse or sudden increases in activity.
- Fat Pad Atrophy: The fat pad in the ball of the foot can thin out, reducing shock absorption and increasing pressure on the metatarsals.
- Tight Achilles Tendon or Calf Muscles: Limited ankle flexibility can alter foot mechanics, leading to increased forefoot pressure.
- Medical conditions: Less frequent causes include inflammatory arthritis conditions, such as rheumatoid arthritis, gout, and neuropathy.
Factors we can influence:
Improper Footwear: This can be a major contributor.
- High heels: These shoes push the metatarsals downward, causing excessive pressure on the forefoot
- Narrow toe box shoes: Shoes that squeeze the toes together can compress nerves and irritate the metatarsal heads.
- Shoes with inadequate support and cushioning: Footwear that doesn’t provide proper shock absorption can exacerbate stress on the ball of the foot.
- Thin-soled shoes
Excess Weight: Extra body weight increases the load on the feet, particularly the forefoot, during walking and standing.
High-Impact Activities: Runners, jumpers, and racquet sport athletes bring repetitive pressure into the forefoot. The constant stress can inflame the metatarsal heads and surrounding tissues.
How to Treat Metatarsalgia
The good news is that most cases of metatarsalgia respond well to conservative treatments. Successful treatment will relieve pain, reduce inflammation, and, most importantly, address the underlying cause.
Conservative, At-Home Treatments:
Rest: Avoid or modify activities that aggravate the pain. This may involve changing or shortening your workout.
Ice: Apply ice packs wrapped in a thin cloth to the painful area for 5-10 minutes several times a day to reduce inflammation and pain.
Pain Relievers: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help manage pain and reduce inflammation. These must be taken with your doctor’s permission to avoid potential medical complications.
Proper Footwear: This is essential to successful treatment
- Choose shoes that fit well and are as wide as your foot.
- Opt for shoes with good arch support and ample cushioning in the forefoot.
- Avoid high heels and shoes with thin soles. Wedge styles will often cause less pressure on the ball of the foot compared with high heels.
- Rocker-soled shoes can help by reducing pressure on the ball of the foot during walking. However, in the long term, they increase the risk of a significant movement range limitation in two out of three axes, resulting in permanent deterioration of the gait path. Hence, they should be used as a temporary relief only.
Metatarsal Pads: These pads are placed in your shoes just behind the ball of your foot. They help to offload pressure from the painful metatarsal heads and redistribute weight. It is crucial that these pads are not placed directly under the metatarsal heads, but slightly behind them, to effectively relieve pressure and avoid worsening the condition.
Insoles: Over-the-counter shoe inserts can help correct biomechanical imbalances, provide cushioning, and support the metatarsals and the arch.
One effective solution is the FootWave METATARSALGIA insole. Designed specifically for forefoot pain, this orthotic provides targeted metatarsal support to unload the painful area, while also stabilizing the midfoot and supporting the arch. The unique shape of the metatarsal dome, combined with shock-absorbing materials and anatomically contoured design, improves foot alignment and reduces pressure in the ball of the foot, making it ideal for both everyday wear and active use.
Calf stretches: Improving ankle flexibility can help reduce forefoot pressure.
Foot stretches and strengthening exercises: Strengthening the muscles within the foot (intrinsic muscles) can create a stronger, more flexible, and better functioning foot.
Weight Management: Losing even a small amount of weight can significantly reduce stress on your feet
Activity modification: Change to activities that put less pressure on the forefoot, change to a more cushioned surface, and /or shorten the workout to alleviate stress in the painful area.
Medical Interventions (If conservative measures don’t provide sufficient relief after a few weeks, your podiatrist may recommend further treatments):
Prescription Medications: Stronger anti-inflammatory medications may be prescribed.
Corticosteroid Injections: Sometimes an injection of a corticosteroid into the painful area can provide significant short-term relief from inflammation and pain. However, these are typically used sparingly to avoid weakening surrounding structures.
Physical Therapy: A physical therapist can provide a tailored program of exercises, stretches, and other modalities to address your specific needs and improve foot mechanics.
Shockwave Therapy: This non-invasive treatment uses sound waves to promote healing in the affected tissues.
Addressing Underlying Conditions: If metatarsalgia is caused by conditions like Morton’s neuroma or stress fractures, specific treatments for those issues will be necessary.
Custom foot orthotics: Custom orthotics help address the altered biomechanics of the foot, which are often a contributing factor to metatarsalgia. A recommended option is FootWave PROFESSIONAL customizable orthotics. These orthotics can be tailored by healthcare professionals to precisely match your foot shape and pressure distribution. They offer advanced support for the transverse arch and metatarsal zone, helping correct postural abnormalities and offload sensitive areas in a controlled, medical-grade way.
Surgical Intervention: Surgery is rarely needed for metatarsalgia and is generally considered only when all other conservative treatments have failed and the pain is debilitating.

Prevention is Key
Several measures can be taken preventively to keep the feet healthy and pain-free:
- Wear appropriate footwear at all times.
- Maintain a healthy weight.
- Stretch your calf muscles regularly.
- Use a quality insole to provide support and cushioning for the feet.
When to See a Doctor
While mild metatarsalgia often resolves with self-care, consult a podiatrist if:
The pain is severe or doesn’t improve after a couple of weeks of home treatment.
The pain worsens or keeps returning.
You experience numbness or tingling in your toes.
You have diabetes and develop foot pain, as foot problems can be more serious.
You’re unsure of the cause of your foot pain.
Metatarsalgia can be successfully treated, allowing you to resume all your activities. Don’t allow metatarsalgia to hold you back from the life you love!
Disclaimer: This article is intended for educational purposes only and does not constitute medical advice. Always consult your physician, podiatrist, or pharmacist before starting any treatment, including over-the-counter medications like NSAIDs. Individual medical needs may vary, and only a qualified professional can provide specific advice.







